Key takeaways from ISPOR Europe Health Economics trends for SaMD
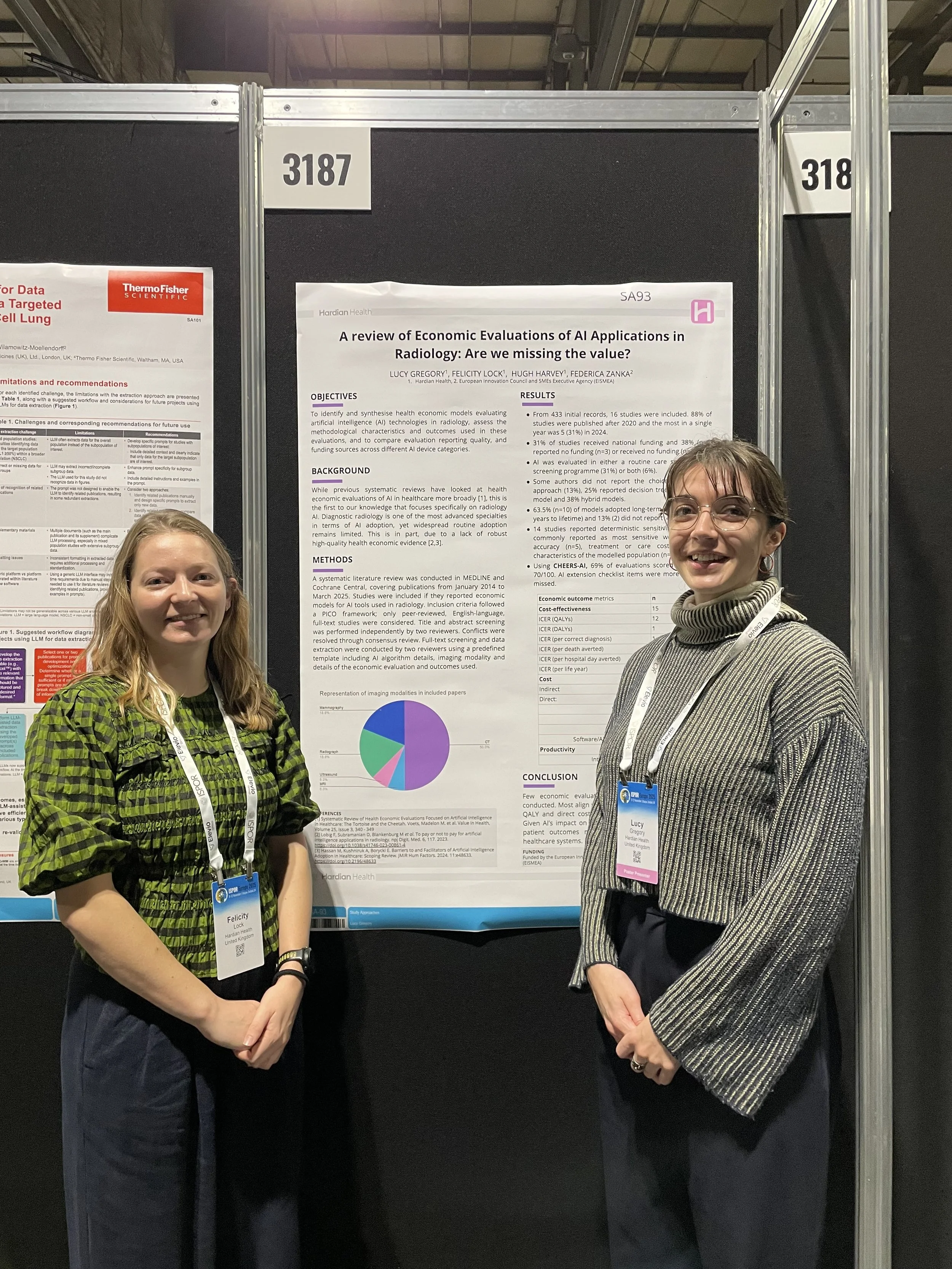
Hardian team members Lucy Gregory (Health Economics Consultant) and Dr Felicity Lock (Senior Clinical Associate) recently returned from ISPOR Europe, an international conference in Glasgow dedicated to Health Economics and Outcomes Research. If ISPOR is unfamiliar territory, this overview explains why it should matter to anyone developing AI and software as a medical device.
What is ISPOR?
ISPOR is the global professional society for Health Economics and Outcomes Research. Founded in 1995, it sets methodological standards, advances best practice, and supports the use of evidence to inform healthcare decision making. Much of the organisation’s historical focus has been on pharmaceuticals but the past several years have seen a clear shift toward medical devices and digital health technologies.
Why ISPOR is increasingly relevant for AIaMD and SaMD
While the clinical adoption of AI and SaMD has progressed slowly in Europe, ISPOR’s work is becoming central to how these products will be evaluated, reimbursed and adopted.
Manufacturers seeking market access for digital health tools will need to engage with HEOR frameworks more closely, particularly as HTA bodies begin to assess these technologies with greater scrutiny.
Medical devices on the ISPOR agenda
The 2025 edition of ISPOR Europe had a number of medical device offerings, here are some of our standout moments:
There were several seminars focusing on modernising medical device evaluation covering a range of topics including aligning life-cycle evidence, Health Technology Assessment (HTA) methodologies for digital tools, and building effective HEOR capabilities for Medical Devices and Diagnostics.
We explored the poster sessions running throughout the event. This included presenting our own poster on the value of Radiology AI, which generated constructive discussions with researchers and professionals working across the SaMD space.
We attended a collaborative meeting between ISPOR’s Digital Health and Medical Devices & Diagnostics Special Interest Groups. It was a great insight into the work going on behind the scenes at ISPOR to progress the field and highlighted the importance of collaboration when developing best practices.
Click here to read our poster
Hardian’s key takeaways
SaMD has a much shorter lifecycle compared to pharmaceuticals
This might seem obvious, but it’s an important point to state up front. Medical devices and pharmaceuticals aren’t the same and trying to apply the same frameworks is challenging. Software devices evolve quickly, update regularly and often rely on iterative improvements (which is frankly one of their major benefits). Therefore, trying to shoehorn SaMD into traditional pharma frameworks is unlikely to be successful.
That doesn’t mean to say there isn’t a wealth of information that can (and will) be gained from the best practices built by the pharmaceutical industry.
Given this short lifecycle, should we be looking at more of a life cycle approach to evidence generation for SaMD?
Dynamic healthcare innovations require dynamic evaluation. There is a growing consensus that having a life cycle approach to evidence generation for software devices could help combat the disconnect between continuously evolving software and the rigidity of regulatory and HTA bodies.
Right now there isn’t enough information to know whether digital technologies provide value for money. The suggestion of using other sources of evidence over traditional RCTs comes up frequently. This could include HTA bodies considering published and unpublished evidence, utilising early economic modelling and increasing focus on real world evidence.
This also raises the need for strong partnerships between manufacturers and healthcare providers to facilitate this continuous safety and performance monitoring. There are also some aspects that are not clear yet, including the consequences of introducing AI into clinical pathways and the impact on wider care and health inequalities.
Cost-effectiveness may not fully capture the value of digital health technologies
Traditionally, healthcare interventions have been assessed only on their cost-effectiveness (i.e. how much benefit do we get for the money we spend). Attendees of the congress recognised that digital health technologies often have a much wider range of outcomes than other healthcare interventions like pharmaceuticals.
However, this is not yet reflected in the outcomes considered for reimbursement i.e. dominance of cost per QALY (aka Quality Adjusted Life Year i.e. how much good and healthy life something provides, where 1 = 1 year in perfect health). This means that we are assuming the direct benefit of digital technologies will be some improvement in patient outcome (i.e. quality of life). While that’s (obviously) not a bad thing, if evaluations focus solely on QALYs, the healthcare system risks undervaluing technologies that improve capacity, safety and workflow reliability. While some of these benefits may eventually show up in terms of QALYs (derived from treatment outcomes), many of them probably won’t.
Health systems are complex, and there are numerous steps along care pathways. For example, with software intended to support the reporting of lung nodules, it could take many years before we know whether the patient lived longer. If we focus too much on QALYs, are we failing to accurately assess a technology’s potential impact?
Shared understanding and communication remain a barrier
The joint meeting between ISPOR’s Digital Health and Medical Devices & Diagnostics Special Interest Groups revealed the recurring challenge that individuals across the community speak different professional languages. This misalignment is particularly common in discussions about regulatory submissions, evidence expectations and how regulatory and HTA processes could work together to avoid duplication.
On that note, where are all the AIaMD and SaMD manufacturers?
One noticeable gap was the absence of SaMD manufacturers. Compared to larger health tech conferences, the presence of innovators was limited. This matters. If best practices are to be realistic and implementable, manufacturers must be part of the conversation.
HTA bodies, regulators, researchers and clinicians cannot develop workable frameworks in isolation. SaMD companies bring practical insight into data availability, development constraints and the operational realities of deployment. Their involvement is essential for ensuring that emerging methodologies reflect what is achievable in practice.
Hardian Health is a clinical digital consultancy focused on leveraging technology into healthcare markets through clinical strategy, scientific validation, regulation, health economics and intellectual property.